Date: April 25, 2025
Attention: All Providers
Effective date: May 1, 2025
Call to action: Texas Children Health Plan (TCHP) would like to remind providers of the in-lieu-of services available to our members.
Texas Children’s Health Plan covers the following HHSC-approved in-lieu-of services as medically appropriate and cost effective settings as an option for our members who choose these services as an alternative level of care to the acute care inpatient hospital setting:
- Partial Hospitalization (PHP)
- Intensive Outpatient Program (IOP)
How this impacts providers: Providers may consider referral to or delivery of partial hospitalization or intensive outpatient program care as an alternative to inpatient acute care when medically appropriate and with the member’s expressed consent upon discharge from inpatient psychiatric or substance use disorder treatment or when outpatient management of mental health conditions or SUD has failed.
- TCHP’s Service Coordination and Utilization Management teams collaborate with providers to ensure in-lieu-of-services are considered, authorized, and coordinated during discharge planning from inpatient hospitalization or when escalating care from the outpatient setting.
- Members are not required to utilize in-lieu-of services or settings instead of a traditional service or setting, but may consider in-lieu-of services as an option when medically appropriate and cost effective.
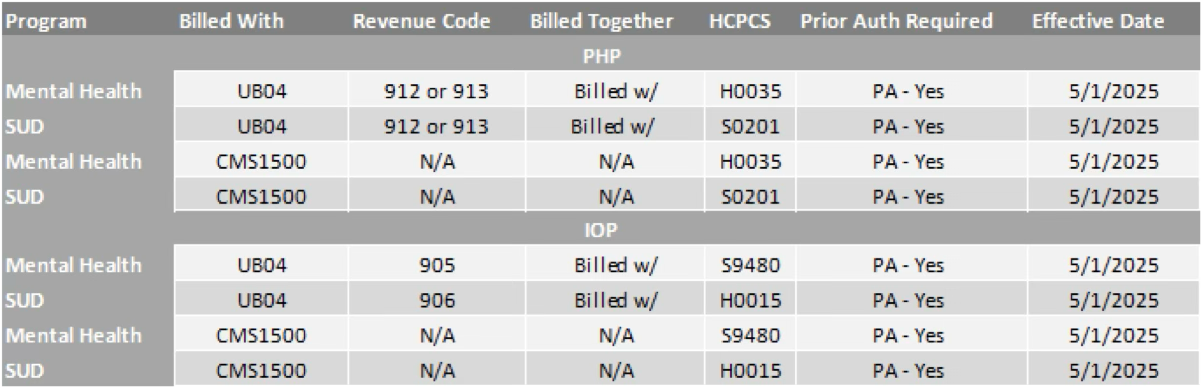
- Partial hospitalization and Intensive Outpatient program care require prior authorization. TCHP covers these services when authorized and billed in accordance with the Partial hospitalization and Intensive Outpatient Program Billing Grid below.
- TCHP will allow leniency in billing requirements as providers adjust through May 31, 2025. Authorized IOP and PHP services billed on a clean claim through 5/31/2025 will be reimbursed. Claim submission for authorized services must comply with the billing requirements in the Partial hospitalization and Intensive Outpatient Program Billing Grid starting 6/1/2025.
Prior Authorization Information
Prior authorization is required for PHP and IOP in-lieu-of-services. Prior authorization requests for in-lieu-of-services can be securely submitted online from the provider portal, Texas Children’s Link, at https://www.texaschildrenshealthplan.org/providers/link-provider-portal.
Or send via fax to 832-825-8767 or toll-free fax line to 1-844-291-7505. Providers should include essential information as required in the UMCM 3.22 and include supporting clinical documentation.
- Partial Hospitalization Program (PHP) - Providers of partial hospitalization services for mental health may include hospital outpatient departments and clinic/group practices enrolled in Medicaid and able to meet the below requirements with a multidisciplinary team approach to patient care under the direction of a physician. Members admitted to a PHP must be under the care of a physician who certifies the need for partial hospitalization services at a minimum of 20 hours per week of therapeutic services, as evidenced by their plan of care. When partial hospitalization is used to shorten an inpatient stay and transition the patient to a less intense LOC, there must be evidence of the need for the acute, intense, structured combination of services provided by a PHP.
- Intensive Outpatient Program (IOP) - Intensive outpatient services are organized non-residential services providing structured group and individual therapy, educational services, and life skills training which consists of at least 10 hours per week for four to 12 weeks, but less than 24 hours per Day. As required in Section 9 (SUD Services) of the Behavioral Health and Case Management Services Handbook (Vol. 2, Provider Handbooks) of the TMPPM, LOC and specific services provided must adhere to current evidence-based industry standards and guidelines for SUD treatment, such as those outlined in the current edition of the American Society of Addiction Medicine’s (ASAM’s) Treatment Criteria for Addictive Substance-Related and Co-Occurring Conditions.
Texas Children’s Health Plan Members must provide written consent to receive in-lieu-of-services. Providers rendering the service obtain Member consent and provide to Texas Children’s Health Plan or HHSC upon request. TCHP will give providers 24 business hours to submit requested consent information.
Reimbursement information
- Reimbursement will align with provider’s existing contract terms.
- Applicable providers will receive an attestation online form from TCHP’s Provider Relations Department for their review and submission. This attestation covers provider qualifications and an agreement to obtain member consent for in-lieu-of services offered. Provider qualifications for In-Lieu-of-Covered Services are defined by the Uniform Managed Care Manual Chapter 16.3 (or its successor).
- All programs listed below require Prior Authorization in order to be reimbursed.
Partial Hospitalization Program (PHP) is available for members with a Mental Health or Substance Use Disorder.
Intensive Outpatient Program (IOP) is available for members with a Mental Health and Substance Use Disorder.
Services are rendered in hospital outpatient departments, community mental health centers, Federally Qualified Health Centers (FQHC), Rural health clinics (RHC), addiction treatment centers and/or private clinics.
- IOP services billed on a CMS 1500 claim form should be billed using:
- Procedure code H0015 (Alcohol and/or drug services; intensive outpatient) OR
- Procedure code S9480 (intensive outpatient psychiatric services)
- H0015 and S9480 will not be reimbursed separately if billed on the same day.
- IOP services billed on a CMS 1450 claim form should be billed using:
- Procedure code H0015 (Alcohol and/or drug services, intensive outpatient) AND revenue code 906 for SUD services
- Procedure code S9480 (intensive outpatient psychiatric services) AND revenue code 905 for mental health services
- H0015 and S9480 will not be reimbursed separately if billed on the same day.
- Providers must obtain a prior authorization to be reimbursed for IOP services.
Partial hospitalization and Intensive Outpatient Program Billing Grid
Next step for Providers: Providers must follow the guidance within this communication and are encouraged to share this information with their staff.
If you have any questions, please email Provider Relations at: providerrelations@texaschildrens.org.
For access to all provider alerts: www.texaschildrenshealthplan.org/provideralerts.
Resources